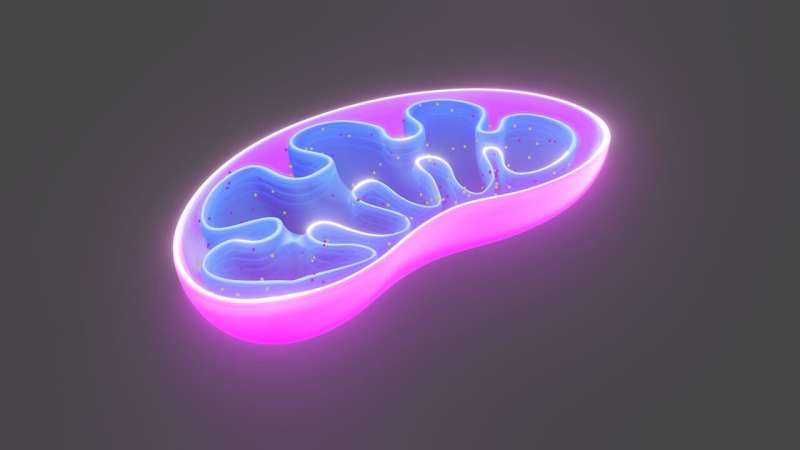
Mitochondria play a crucial role in cellular energy production, which is essential for the proper functioning of various cell types. Recent research has unveiled a significant connection between mitochondrial dysfunction and the pathogenesis of type 2 diabetes. This article explores the underlying mechanisms of mitochondrial damage in diabetes, proposes potential therapeutic strategies, and discusses implications for future research.
The Connection Between Mitochondrial Function and Diabetes
Type 2 diabetes is characterized by insulin resistance and inadequate insulin secretion, resulting in elevated blood glucose levels. The insulin-producing pancreatic β-cells exhibit mitochondrial defects, which hinder their ability to generate sufficient energy. According to a study published by researchers at the University of Michigan, abnormal mitochondrial activity in these β-cells leads to a cascade of cellular responses that impair their maturation and function.
"We wanted to determine which pathways are important for maintaining proper mitochondrial function." – Emily M. Walker, Ph.D.
Key Findings
- Mitochondrial dysfunction in pancreatic β-cells compromises insulin production.
- Damage to mitochondrial DNA triggers a stress response that prevents β-cells from maturing.
- This dysfunction is not isolated to β-cells; liver and adipose tissue cells also exhibit similar mitochondrial defects under diabetic conditions.
Mechanisms of Mitochondrial Dysfunction
The research team damaged three critical components of mitochondrial function, which included:
- Mitochondrial DNA: Damage to this DNA impairs the mitochondria's ability to produce necessary proteins.
- Quality Control Pathways: These pathways are essential for eliminating dysfunctional mitochondria.
- Mitochondrial Biogenesis Pathways: These pathways maintain a healthy population of mitochondria within the cell.
| Component | Impact of Damage |
|---|---|
| Mitochondrial DNA | Impaired energy production leading to cell dysfunction. |
| Quality Control Pathways | Accumulation of damaged mitochondria and heightened stress response. |
| Mitochondrial Biogenesis | Failure to increase mitochondrial numbers in response to energy demands. |
Potential Therapeutic Approaches
One promising avenue explored in the study is the use of a drug called ISRIB, which targets the protein synthesis pathways affected by mitochondrial dysfunction. Treatment with ISRIB allowed β-cells in mice to regain their capacity to regulate glucose levels effectively.
Study Implications
The implications of these findings extend beyond just pancreatic β-cells. Given that mitochondrial dysfunction was also observed in liver and adipose cells, this suggests a systemic impact of mitochondrial health on diabetes management:
- Restoring Mitochondrial Function: Targeting mitochondrial health could represent a new therapeutic strategy for diabetes.
- Broader Applicability: The research opens pathways for investigating mitochondrial roles in other tissues affected by diabetes.
Future Directions in Research
Continuing research is vital to unravel the complex interactions between mitochondrial dysfunction and diabetes. Future studies could focus on:
- Identifying additional cellular mechanisms influenced by mitochondrial health.
- Testing the efficacy of ISRIB and similar compounds in human cell models.
- Exploring the relationship between lifestyle factors, such as diet and exercise, and mitochondrial function in diabetic patients.
Enhanced understanding of these pathways may lead to significant advancements in diabetes therapy, providing hope for patients seeking effective treatments based on the root causes of their disease.
References
Emily M. Walker et al. Retrograde mitochondrial signaling governs the identity and maturity of metabolic tissues, Science (2025).
Lifespan.io












Discussion