Recent research conducted by the Dana-Farber Cancer Institute has shed light on the efficacy of donor lymphocyte infusion (DLI) as a treatment for patients with acute myeloid leukemia (AML) who experience relapse following an allogeneic hematopoietic stem cell transplant. The study, published in Science Immunology, identifies critical factors that influence the likelihood of remission following this treatment.
Understanding Acute Myeloid Leukemia
AML is a complex and aggressive form of blood cancer, characterized by the rapid proliferation of myeloid cells in the bone marrow. While allogenic hematopoietic stem cell transplants can potentially offer a cure by introducing healthy donor cells into the patient, approximately one third of AML patients experience relapse post-transplant.
The Role of Donor Lymphocyte Infusion
DLI is a therapeutic strategy designed to combat such relapses by infusing lymphocytes, a type of white blood cell, from the stem cell donor into the patient. This procedure aims to leverage the immune power of the donor's cells to recognize and attack remaining leukemia cells, a phenomenon known as the graft versus leukemia effect.
Challenges with DLI
Despite its promise, DLI only achieves success in about 15-20% of relapsed AML patients. Dr. Katie Maurer, the first author of the study, emphasized the need for a deeper understanding of the underlying mechanisms that determine DLI success, as outcomes after relapse are typically poor.
Research Methodology
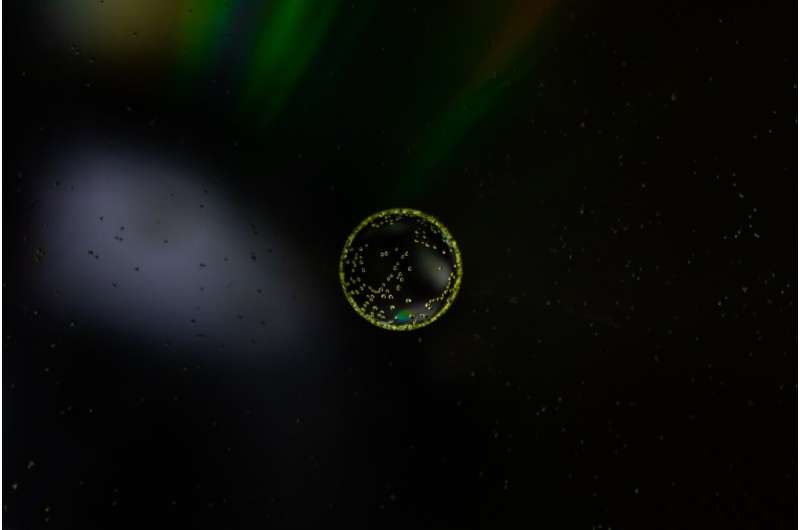
The research team examined the bone marrow samples from 25 patients with relapsed leukemia who received DLI. By employing single cell sequencing, they were able to analyze the distinct populations of cells present in each patient's bone marrow and assess how these populations influenced immune responses.
Key Findings
The analysis revealed significant differences in the cellular compositions between patients who responded to DLI therapy and those who did not. These findings suggest that some forms of AML may be classified as either “hot” or “cold,” analogous to the immunogenic characteristics observed in solid tumors:
- Hot AML: Responsive to immune therapies.
- Cold AML: Less likely to respond to immune therapies.
Crucial Immune Cell Identified
One of the pivotal breakthroughs of this research was the identification of a specific immune cell type linked to DLI success—CD8+ cytotoxic T lymphocytes that express the transcription factor ZNF683/Hobit at high levels. This subset appears to coordinate immune responses and directly target leukemia cells.
| Cell Type | Characteristics | Role in DLI Response |
|---|---|---|
| CD8+ Cytotoxic T Lymphocytes | High levels of ZNF683/Hobit expression | Coordinate immune attack against leukemia cells |
| Inactive T Cells | Low ZNF683/Hobit levels, higher inhibitory markers | Reduced effectiveness in targeting cancer cells |
Implications for Future Therapies
Dr. Maurer articulated the significance of these findings by stating that understanding the mechanisms behind patient responses to DLI can pave the way for the development of more effective T cell therapies for AML. By targeting the identified CD8+ T cells and optimizing their function, researchers hope to enhance the effectiveness of DLI for a broader patient population.
“The goal of our research is to identify the ways in which some patients respond, in the hopes that uncovering these mechanisms can help us create improved therapies that are more effective for a greater number of patients.” – Dr. Katie Maurer
Conclusion
These findings represent a significant advancement in the understanding of cellular therapies for AML, illuminating key factors that influence patient outcomes. As research continues, the identification of immune cell dynamics will play a crucial role in developing enhanced therapeutic strategies for treating this challenging disease.
Further Reading
For a deeper exploration of this topic, refer to the original study: Maurer, K. et al. "Coordinated immune networks in leukemia bone marrow microenvironments distinguish response to cellular therapy," Science Immunology (2025).













Discussion